Overview and a Question
Early next year, the legislature will likely continue efforts to address the rising dysfunction, disability and death from opioid drug abuse. The Senate passed a bill this fall which is under consideration by the House. The Governor has also filed legislation and the House will likely have a bill of its own. Hopefully, we will be able to take the best elements of those bills to craft a final package. Meanwhile, the legislature and the administration are addressing many dimensions of the problem through other legislative vehicles and existing executive powers.
Focusing first on addiction to prescription pain killers, I wanted to pull statistics together and to get your local perceptions on the issue. You can wade through the numbers below, but I’ll offer my summary observations here:
- We face three intertwined problems:
- Casual, episodic youth abuse of pain killers with potentially tragic consequences. Thrill-seeking kids now have easy access to potentially fatal substances.
- Opioid/heroin addiction of young people, whether through a surgical or injury experience or, perhaps more commonly, just through continued risky abuse in a detrimental peer group.
- Older individuals with chronic conditions who may use or abuse pain relievers prescribed to them and perhaps make fatal mistakes using them in combination with other drugs like alcohol and benzodiazepines.
- An additional category of opioid users is cancer patients in hospice settings, where the only real issue is to protect them from pain.
- The problem of episodic youth abuse may be peaking and turning down as awareness builds as to the risks of pills.
- The problem of addiction and overdose among young adults is at its highest level ever and may not have peaked. The harms associated with addiction have been multiplied by the introduction of fentanyl into the illicit markets.
- There is a lot of evidence that doctors are getting the balance between pain control and addiction control wrong and letting too many pills out into the environment, but there are two sides to that story.
Based on what you are seeing and hearing yourself, are doctors you know getting the balance wrong and making pain medication too readily available? If they are getting the balance wrong, there is a second and distinct question: do you feel that the legislature should pass new laws regulating the decisions that doctors make with patients? I’m most interested in personal experiences, but also very interested in any reliable data sources that I should add to the collection below.
You can comment at the end of the article: Feel free to comment without using your full name if you prefer to remain anonymous. I’d very much welcome comments from physicians and other health care professionals.
Opioid Overdose Statistics
Recent data from the Center for Disease Control show that:
- In 2014, more people died in the United States from drug overdoses than in any previous recorded year.
- 47,055 died of drug overdoses — while only approximately 30,000 died in motor vehicle crashes.
- The national age-adjusted rate of drug overdose death more than doubled from 2000 to 2014 — from 6.2 per 100,000 people to 14.7 per 1000 people.
- The age-adjusted death rate in Massachusetts, 19.0 deaths per 100,000, was well above the national average.
- Opioid drugs — drugs that are derived from or act in the same way as opium, for example, heroin, fentanyl and oxycontin — were known to be involved in 61% of overdose deaths.
The breakdown underneath the national totals in the CDC report is as follows:
- The age group with the highest drug overdose rate is persons 45-54 years old, with 28.2 deaths per 100,000. Drug poisonings and suicides are driving an overall rise in mid-life mortality among middle-aged white non-Hispanic men and women (after decades of declining death rates).
- Youth aged 15-24 have a death rate that is considerably lower — 8.6 deaths per 100,000.
- People over 25 accounted for over 90% of the deaths.
- Men have a higher death rate than women — 18.3 vs. 11.1.
- Non-Hispanic whites have a death rate (19.0) that is much greater than the rates for Hispanics (6.7) and non-Hispanic Blacks (10.5).
The CDC notes that:
The 2014 data demonstrate that the United States’ opioid overdose epidemic includes two distinct but interrelated trends: a 15-year increase in overdose deaths involving prescription opioid pain relievers and a recent surge in illicit opioid overdose deaths, driven largely by heroin. . . . [I]llicit fentanyl is often combined with heroin or sold as heroin. Illicit fentanyl might be contributing to recent increases in drug overdose deaths involving heroin. Therefore, increases in illicit fentanyl-associated deaths might represent an emerging and troubling feature of the rise in illicit opioid overdoses that has been driven by heroin.
In Massachusetts, unintentional opioid overdose deaths have occurred in almost every community over the past three years. Opioid overdose deaths, 80% of which are unintentional, have grown by a factor of 8 over the past 25 years. Unintentional opioid deaths roughly doubled from 2000 to 2013. The demographics of opioid deaths in Massachusetts are similar to the national demographics — tilted to towards people who are middle-aged, white and male and more prevalent than motor vehicle deaths — see Tables 18 and 19 in this death analysis from the Department of Public Health. Local anecdotes that I hear as a legislator also point towards a heavy role for fentanyl and fentanyl/heroin combinations in the recent spike in overdose deaths.
Surveys of Substance Use Prevalence
According to the National Survey on Drug Use and Health, the number of people admitting past-month use of pain-relievers has remained fairly stable for the last decade, bouncing around 2% of respondents (actually dropping slightly in 2013). The rate of admitted past-month heroin use was lower, 0.3% among young adults in 2013, but the rate of heroin use use appears to be rising to levels perhaps twice those reported early in the century.
The count of heroin users reported in the survey is a soft guess, likely a significant underestimate — typically survey methods are less likely to reach people whose lives have become chaotic. Alternative measurements of cocaine use prevalence suggested rates far above those detected by surveys in a study I did in the 90s. However, the divergence in trends (between prescription drugs and heroin) is meaningful and consistent with the divergence in trends in the death statistics.
While deaths from prescription drug overdose are higher among middle-aged adults than among young adults, more young adults (18 to 25) admit past month non-medical use of “psychotherapeutics” — the category that includes pain relievers — than older adults: 4.8% as compared to 2.1%. But the young adult rate was lower in 2013 than the rates from 2002 to 2010.
The number of first time users of non-medical psychotherapeutics dropped significantly in 2013 to 1.539 million — the peak year in the past decade was 2003 with 2.456 million initiations. The rate of initiation is a leading indicator, so this drop is encouraging. The 2013 Massachusetts Youth Risk Behavior Survey, administered confidentially in schools, shows drug use flat to down in most categories. However, non-medical use of prescription drugs is still second only to marijuana as measured by life-time experience among high school students (41% vs. 13% vs. single digits for other kinds of drugs).
Also perhaps encouraging are the leveling-off in the rate of persons meeting criteria for dependence on or abuse of pain relievers — see the Household Survey at Figure 7.3 — and the drop in illicit drug dependence among youths aged 12 to 17 (Figure 7.5). This coincides with an increase in the rate of people receiving treatment for pain relievers (Figure 7.9).
One way of reading these data is that, overall, fewer people are initiating abuse of pain relievers and the trend may be positive, but there is an increasingly visible sub-population that is continuing to use, turning to heroin, feeling the need for treatment and overdosing on fentanyl-laced street drugs.
Health Care Events
Treatment data are hard to interpret because drug treatment program admissions reflect both need and availability. Availability may be more stable than need, so stability in treatment admissions may be as much related to limited availability as to need. With that caveat, treatment statistics from the Massachusetts Bureau of Substance Abuse Services, show the following:
- Overall admissions were stable at about 100,000 per year from 2005 through 2014.
- In the same period, heroin admissions rose as a share of overall admissions, from 38.2% to 53.1%, while alcohol and cocaine admissions fell.
- Admissions for opioids other than heroin peaked at 10.9% in 2011 and dropped backed to their 2005 level of under 6% by 2014.
- Youth admissions (under 18) trended slightly down from 2004 to 2012. For most youth (72.2%) marijuana or alcohol was the primary substance of abuse, but 14.8% reported having used heroin in the past year and 33.2% reported having used other opioids in the past year.
- Admissions for older adults (over 55) trended distinctly upward from 2003 to 2012. Alcohol was the primary drug of abuse in 71.4% of the admissions, but 17% were admitted for heroin abuse and 9.2% had used other opiates in the past year.
Emergency room admissions are less constrained by supply and do show increases in the period from 2004 to 2011. Boston-area emergency rooms report to the federal Drug Abuse Warning Network. Emergency room visits in the Boston-Cambridge-Quincy Metropolitan Statistical Area show the following trends:
- Overall, emergency room visits for substance abuse rose 41% from 2004 to 2011 — 35% among persons 21 to 24, 97% among persons 45 to 54.
- The total number of emergency room visits was estimated at 51,845 in 2011 or roughly 1 for every 100 persons in the area (although many visitors may have repeated, so the true share of people with a visit to the emergency room for substance abuse is probably lower).
- Mentions of cocaine use (12,562) were only slightly below heroin mentions (14,057) in 2011; both categories trended upwards from 2004 — cocaine mentions by 34%, heroin mentions by 37%. The 2011 data do not capture the recent spike that has been so much in the news.
- Mentions of opiates/opioids were up 68% in the period, reaching 9,354 in 2011.
- Benzodiazepines (anti-anxiety drugs like valium) were also up 66%, reaching 8,725 in 2011, close behind the pain relievers.
This last finding highlights the risks of polysubstance abuse. Rhode Island’s Strategic Plan on Addiction and Overdose examined the concurrent use of substances resulting in overdose deaths, finding that benzodiazepines were frequently present together with cocaine, heroin and/or fentanyl.
Prescription Drugs
There is little debate as to whether increased prescriptions by doctors of opioids for pain have contributed to addiction and overdoses. I have heard countless stories of people who have received prescriptions for large quantities of narcotics after relatively minor procedures. They are then faced with the question of how to dispose of them. I have a friend whose child got in trouble for bringing to school pills left over from a surgical procedure and attempting to sell them.
In her testimony to Congress on May 14, 2014, the head of National Institute on Drug Abuse, said:
Several factors are likely to have contributed to the severity of the current prescription drug abuse problem. They include drastic increases in the number of prescriptions written and dispensed, greater social acceptability for using medications for different purposes, and aggressive marketing by pharmaceutical companies. These factors together have helped create the broad “environmental availability” of prescription medications in general and opioid analgesics in particular.
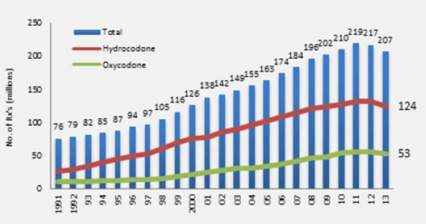
The figure below, taken from the same testimony shows opioid prescriptions dispensed by US retail pharmacies almost tripling from 1991 to 2011, although dropping slightly over the last year or two.
To put these quantities in perspective, in 2010 enough opioid pain relievers were sold in the United States to “medicate every American adult with a typical dose of 5 mg of hydrocodone every 4 hours for 1 month.” Put that another way, enough pain relievers were sold to keep 1 in 12 adults medicated on a year round basis. Geographic and demographic variations in prescription rates correlate roughly with overdose death rates.
The Governor’s Working Group on opioids cited a telling statistic from the National Survey on Drug Use and Health in 2013:
Source Where Pain Relievers Were Obtained for Most Recent Nonmedical Use among Past Year Users Aged 12 or Older: 2012-2013
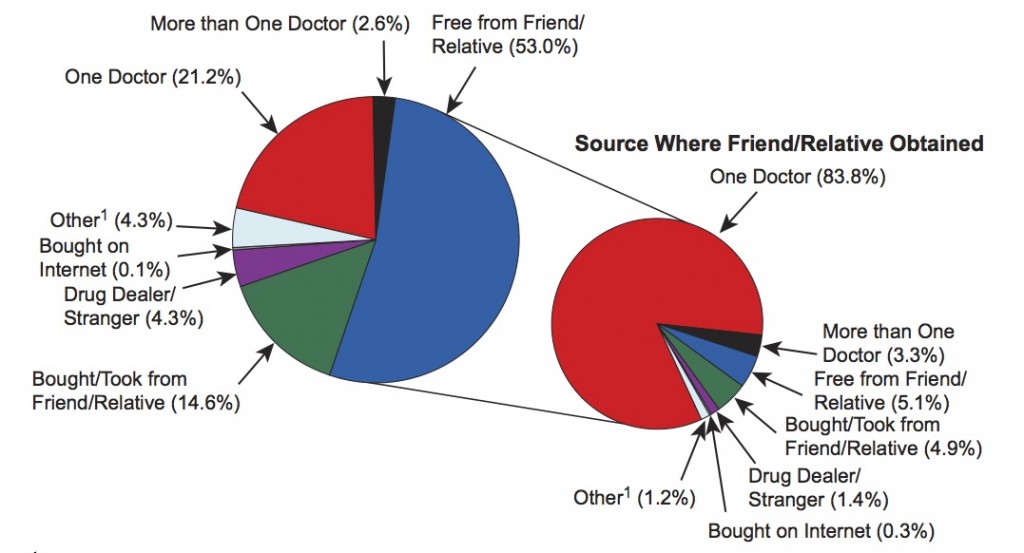
This chart shows that very few people using pain relievers non-medically got them from strangers or dealers (only 4.3%). Some got them directly from doctors but most got them from friends or relatives who, in turn, in 83.8% of cases, got them from one prescribing doctor. These survey results apply to the whole universe of people who have used opioids in the past year and therefore includes many who use is only casual. Another study reached a different conclusion as to the sources of drugs for people actually diagnosed with opioid abuse or dependence: 79.9% had an opioid prescription of their own prior to their first abuse diagnosis. But either way, the source of abused opioids is prescriptions.
An equally telling statistic from the National Survey is that among the 2.8 million people who used drugs illicitly for the first time in 2013, over 20% started with nonmedical use of prescription drugs, 12.5% with pain relievers — marijuana is the most common first drug, but many people go straight to pills. A further stunning statistic consistent with a perception that there are just too many pills out there accessible to kids — not only opioids, but other abusable psychoactive drugs — was that 12 and 13 year-olds were more likely to admit using pills nonmedically in the past month (1.3%) than marijuana (1.0%) — Figure 2.8 in the National Survey. Another study that the Governor’s working group cited indicates that “[A]dolescent males who participate in sports may have greater access to opioid medication, putting them at greater risk to misuse these controlled substances.”
A CDC analysis in 2012 showed that how widely prescription rates vary across the states, tending to suggest differing approaches to main management. Massachusetts compares as follows:
- Low in its overall prescription rates for opioid pain relievers, ranking 41st in prescriptions compared to populations.
- Low in prescribing high dose pain relievers, ranking 41st.
- High in long-acting, extended-relief opioids like Oxycontin, ranking 8th among the states.
- High in benzodiazepines, ranking 9th among the states.
That CDC analysis concludes:
Factors accounting for the regional variation are unknown. Such wide variations are unlikely to be attributable to underlying differences in the health status of the population. High rates indicate the need to identify prescribing practices that might not appropriately balance pain relief and patient safety.
The Pain Control Movement
As clear as it is that pain medications are a precipitating factor for the surge in addiction, there is also a powerful movement to control pain better. In fact, in section 4305 of the landmark Patient Protection and Affordable Care Act, Congress ordered the Department of Health and Human Services to convene a conference with the following purposes — to:
(A) increase the recognition of pain as a significant public health problem in the United States;
(B) evaluate the adequacy of assessment, diagnosis, treatment, and management of acute and chronic pain in the general population, and in identified racial, ethnic, gender, age, and other demographic groups that may be disproportionately affected by inadequacies in the assess-
ment, diagnosis, treatment, and management of pain;
(C) identify barriers to appropriate pain care;
(D) establish an agenda for action in both the public and private sectors that will reduce such barriers and significantly improve the state of pain care research, education, and clinical care in the United States.
The Institute of Medicine convened a distinguished panel in response to this order. Their report brief dated June 2011, defines pain as a problem affecting 100 million people in the United States and costing $635 billion per year. It uses the same kind of ambitious language used by groups seeking to address drug abuse use, but focuses on pain as the problem:
Pain represents a national challenge. A cultural transformation is necessary to better prevent, assess, treat, and understand pain of all types. Government agencies, healthcare providers, healthcare professional associations, educators, and public and private funders of health care should take the lead in this transformation. Patient advocacy groups also should engage their diverse constituencies.
In comments delivered to the panel, pain patients lamented their treatment as criminals and physicians prescribing opioids complained of unfair scrutiny. The federal panel’s full report spoke of access to opioids for pain as a human right.
A reasonable degree of access to pain medication—such as the stepped approach of the World Health Organization’s Pain Relief Ladder for cancer—has been considered a human right under international law since the 1961 adoption of the U.N. Single Convention on Narcotic Drugs (Lohman et al., 2010; WHO, 2011). Similarly, countries are expected to provide appropriate access to pain management, including opioid medications, under the International Covenant on Economic, Social, and Cultural Rights, which guarantees “the highest attainable standard of physical and mental health” (citation omitted).
The full report does recognize the “conundrum of opioids” as an “underlying principle”, but views it as a manageable problem:
The committee recognizes the serious problem of diversion and abuse of opioid drugs, as well as questions about their long- term usefulness. However, the committee believes that when opioids are used as prescribed and appropriately monitored, they can be safe and effective, especially for acute, postoperative, and procedural pain, as well as for patients near the end of life who desire more pain relief.
The committee viewed opiate abuse as a nuance of pain treatment. Even though the committee devotes a full chapter to pain care and does touch on the issues of diversion and abuse, its recommendations related to pain care focus entirely on removing barriers to treatment, not on reducing abuse. Its overall recommendations seek to encourage greater awareness and treatment of pain as a public health problem. The Massachusetts Pain Initiative is a local organization devoted to those goals which has expressed reservations about both the Senate’s bill and the Governor’s bill that would restrict access to opioids. For more statements and studies on the pain issue, see Drug War Facts.
Consistent with a national effort to treat pain better, the federal government’s hospital care quality survey includes pain management as a metric. Consumers can compare hospitals on a federal website based on the what percentage of patients reported that “their pain was ‘Always’ well controlled”. The pain questions also factor into a federal 1 to 5 star rating system for the patient experience of care in hospitals. In a recent conversation with a hospital administrator, I heard frustration that this system pushes hospitals to use powerful pain medication to get “smiley faces”.
The Governor’s Opioid Working Group, in its June 2015 report, included training for “all practitioners” as to “addiction and safe prescribing practices” as a key strategy. The Massachusetts Medical Society promptly, in August 2015, updated its guidelines for Opioid Therapy and Physician Communication. In October 2015, the Board of Registration in Medicine incorporated these guidelines into new standards of care motivated by the Working Group’s findings.
Summary and Question
Clearly, physicians who are called upon to treat pain face powerful conflicting goals and incentives. Pain is a real problem and addiction is a real problem. Based on what you are seeing and hearing yourself, are doctors getting the balance wrong and making pain medication too readily available? If they are getting the balance wrong, there is a second and distinct question: do you feel that the legislature should pass new laws regulating the decisions that doctors make with patients? I’m most interested in personal experiences, but also very interested in any reliable data sources that I should add to the collection above.
Feel free to comment without using your full name if you prefer to remain anonymous. I’d very much welcome comments from physicians and other health care professionals.
Responses to comments, December 24, 2015
Thanks to all who have weighed in so far — I have read the comments carefully. Here is what I heard:
- A number of people offered examples of receiving much more pain relievers than they needed after simple procedures. It seems clear that there has been a pattern of this. While the need for pain medication is very real in some cases, the pain movement did manage to overshoot, especially when combined with the pressures of satisfaction rating systems and pharmaceutical marketing. The answer to the first question about whether doctors have been getting the balance wrong is “yes, in many instances, but they may be making an adjustment.”
- Other people offered examples of having a hard time getting the pain medications that they legitimately need. It seems clear that this also happens and may happen more in the future. And I hear the point that managing pain and medication can be very complicated and that the idea of “balance” is an oversimplification. It is much harder to judge how often too much medication has been offered in chronic pain cases. This ties broadly to the issue of over treatment generally, very hard to judge — doctors have tools and they may like to use them too much, but those tools can do great good.
- Overall, in this thread of comments, the answer to the second question about whether we should pass new prescription laws is much less clear, but tilts towards “no, don’t interfere in the doctor patient relationship.” I hear some mistrust of doctors (too influenced by big pharma), but more mistrust of government — too likely to put in place clumsy new rules that will help in some cases, but hurt in others.
My sense of the issue is that doctors are under a lot of pressure. Clearly, the Massachusetts Medical Society is responding aggressively with education measures. All too often in the history of drug regulation, by the time we pass new laws, society has already solved the problem in other ways.
Given the current severity of the epidemic and the elevation of public concern, we in the legislature inevitably will pull every lever we can reach, including additional regulation of prescriptions. That is what we always do, for better or for worse — we respond. My goal will be to make sure that the voices of physicians and patients are heard, along with the voices of those who have lost loved ones to addiction, and that the legislation is framed as sensitively as possible to both groups of concerns.
Legislative Progress Update, January 11, 2015
The House is bringing to the floor an updated substance abuse bill. The approach in this bill is very moderate — essentially encouraging doctors to limit prescriptions to seven days, but allowing them latitude to go further if they record the reasons behind their professional judgment to do so. This seems likely a sensitive and realistic approach.
Section 19D. (a) When issuing a prescription for an opiate to an adult patient for the first time, a practitioner shall not issue a prescription for more than a 7-day supply. A practitioner shall not issue an opiate prescription to a minor for more than a 7-day supply at any time and shall discuss with the parent or guardian the risks associated with opiate use.
(b) Notwithstanding subsection (a), if in the professional medical judgment of a practitioner more than a 7-day supply of an opiate is required to stabilize the patient’s emergency medical condition, or the opiate is prescribed for chronic pain management, pain associated with a cancer diagnoses or for palliative care, then the practitioner may issue a prescription for the quantity needed to stabilize the patient’s condition. The condition triggering prescription of an opiate for more than a 7-day supply shall be documented in the patient’s medical record and the practitioner shall indicate that a non-opiate alternative was not appropriate to address the emergency medical condition.
The Senate Chair of the Mental Health and Substance Abuse Committee has commented favorably on the proposal. This more moderate approach is likely to be the way we end up going, but there will be several additional steps of this process before an approach is finalized.
The head of the Massachusetts Medical Society was quoted in the State House News on January 11 as follows:
“I think it’s fair to say we recognize there are too many opioids circulating in the community at large. One of the ways to address that is to take a look at the volume of prescriptions at the front end. We think that looking at a seven-day initial limit as was mentioned in this bill is a reasonable compromise.”
Additional thoughts welcome!

I do think that doctors are making them too readily available. My spouse was in a community hospital recently for an anxiety attack. On the way out the door, the ER called in a prescription for 10 ativan pills- each dose is like a quarter of a pill. so 20-40 doses of a highly addictive drug. This should not be the case. A lower class drug (like xanax) should have been prescribed first and only in a 1 or 2 dose in case of emergency prescription. They should have been told to get follow up from their PCP and get any additional drugs from them. Now my spouse a professional and a non drug using person who was seeking medical help- now has a problem with the medication where I greatly fear they are becoming dependant. They never should have been prescribed that much in the first place. So my inpout would be that the painkillers only prescribed in a minimal dose- like one or 2 doses.
Sorry, but, I can’t offer much in the way to help resolve this major, major problem. Because I don’t have enough time to read and familiarize myself with the wealth of info that you provided, for the time being, the best that I can say presently, would be to continue to leave this problem in the hands of the medical profesion, as it has been. They, as a group, would be more privy to the drug’s nature and the risks associated with the mortality of opiates and other drugs that might be equally dangerous.
Your going after the wrong type of drug – although pain medication may be over prescribed – I think we need to let the medical profession take the lead on qualifying Doctors. Psychopharmacuiticals which are far more dangerous than pain medication needs to be better regulated – too many PCP’s prescribe with out proper instructions to the paitent and follow up. Did you know that most of the mass shootings have been from people on this type of medication. In fact if you look you will see this is a much bigger issue.
Rather than requlate pain medication – which the state is not qualified to do. Dr. be certified to prescripe certain medication – too many over doeses pull the right to prescribe the drug. Or let the FDA and Drug enforcement agency develop the laws – we have bigger issues like DCF to deal with
There should definitely be more oversight of how doctors are prescribing these medications. My personal experiences are not recent enough to be helpful, i think, but they made a big impression on me. For a DSS investigation, I was sent a 72-page fax by CVS of the many prescriptions for pain meds a mother had received from CVS alone and the investigation was because she was claiming migraines on behalf of her 11 year old daughter but not following up on further evaluation. My other experience was being prescribed pain meds after a car accident in 1981, more than I needed, and if I didn’t have a relative who is a doctor who told me of the risks, I would never have known, feel like I could easily have gotten addicted.
Last year I had a wisdom tooth removed and was prescribed hydrocodone acetaminophen for pain relief. Apparently hydrocodone is a narcotic. I received a dozen pills and took one pill but could probably have done without it. Then the issue was what to do with the remaining pills. (I ground them up in used coffee grinds.)
The point is I was prescribed a narcotic painkiller that I did not really need.
My daughter had a surfing accident in Hawaii a few years ago and she was prescribed vidocan …far more than she needed. She threw away the excess pills.
Why this excess prescription of such pain killers? Do the pharmaceutical companies push selling more than needed quantities of such drugs?
As always, I’m happy that you’re in our legislature, even if I don’t live in your district these days!
I’ve been following this issue more closely in the last 18 months as Arlington’s public safety team has sounded the alarm. Your report gave me some new insight, and didn’t significantly contradict my understanding of the problem.
I think the balance has been wrong, particularly on the first-incident level. OK, you got your wisdom teeth out, but you don’t need that 60-day supply. 5, or 3, renewable by a phone call, is just fine. I think the jawboning being done by public safety will make a big difference.
It’s less clear to me that there is a legislative solution. If you’re going to do something, aim at the bad doctor who doesn’t get it. The doctor with really high prescription rates. The trick will be sorting through the ones that have high rates for a good reason.
From one experience, in which the patient was a biomedical scientist, the physician clearly estimated the judgment of the patient correctly, and got the balance just right. But this was a “top” physician and a sophisticated patient. How does one devise regulations that correctly match our confidence (or lack thereof) in the judgment of prescribing physicians?
Will, I am deeply concerned that doctors over-prescribe medications and that they may have financial incentives to do so that they are not disclosing. It is a serious problem that the majority of doctors have financial agreements with drug companies. These medications, in turn, are often paid for by insurance premiums, which affects us all. The rise in prescription drug use is undoubtedly a factor in the huge burden that medical costs now have on our economy. The conflict of interest that many doctors do not disclose is well-documented:
http://www.npr.org/sections/health-shots/2013/12/14/250714833/before-the-prescription-ask-about-your-doctors-finances
I’m not intimately familiar with the particulars of opioids, but I have had personal experience with doctors handing me prescriptions for Vicodin and other drugs without me asking. And I generally don’t fill them unless I absolutely need to. Because I generally do not trust the safety of synthetic drugs, most of which have side effects that are mentioned as after thoughts but can be serious.
There is substantial evidence that over-prescription is taking place, especially with statin drugs (http://healthimpactnews.com/2014/the-cholesterol-drug-war-abc-australia-bans-documentary-exposing-statin-drug-scandal/). We as a society will bankrupt ourselves if we don’t shift our focus and financial incentives to preventive care and wellness, instead of relying on pills to solve every health problem. Undoubtedly there are instances where prescriptions are necessary, but most cases are preventable.
Follow the money!
After reading the article on drug use and deaths, I strongly support the governor’s plan to limit prescriptions to 3 days of pain killers after a procedure. Seems like only small quantities should ever be dispensed unless some control and accountability are included and assurance that the household doesn’t have others who could use the pills also. The hassle it adds to those in pain could significantly reduce the availability of pills for others to abuse.
I can give you two examples of when I personally was over-prescribed opioids. That said, I’m AGAINST laws that further intrude into the doctor – patient relationship. Give the doctors more training in this area, but don’t artificially limit them to giving a certain number / amount of drugs. To do that assumes the same medication is needed for a sprain or a major surgery. It also treats people like they all have the same pain tolerance.
There is no law that you can write that will cover all cases, so unless you are willing to go to medical school, leave these decisions to those who have. Instead, make sure the doctors are getting the right training and then get out of the way and let them do their jobs.
Finally, I don’t see any mention in the role of pharmacists in this discussion. My brother-in-law is a pharmacist, and he is constantly complaining about the lack of drug knowledge exhibited by doctors. Maybe there is a role here for the pharmacists to play?? Or maybe opioids that are prescribed should be in a database like the Sudafed type drugs. That database makes having allergies a PIA, but it seems to work for the problems they cause.
Reports about pharmaceutical drug reps have shown that doctors rely on what the drug reps tell them. Doctors, despite their good intentions, don’t have the time to do their due diligence about all the drugs that are out there. The problem, in my opinion, is that the information about drugs is coming straight from those who have a financial interest in selling a product. And doctors often have a financial incentive to prescribe. Yes, let’s not interfere with doctor-patient relationship. But in my opinion, there needs to be more oversight of relationships between drug companies and doctors.
Yes — we do have a database for use opioid drugs.
70% of Americans are routinely taking at least 1 prescription drug. How has this become normal and acceptable? People who are healthy should not need any prescription drugs. Either the majority of people are unhealthy, or there’s some serious over-prescription going on, or both. Either way, we need to do something to bring these numbers down. John Oliver has a very good segment about this:
https://www.youtube.com/watch?v=YQZ2UeOTO3I
Love this segment, which I had not seen. Echoes Jim Recht’s points above. Thanks, Sam.
Any time someone in my family has had a surgery, we always got more pain meds than we needed. I’d rather get fewer pills with the ability to get more in a couple of days.
That doesn’t seem to require legislation. It seems more like it requires common sense, or a change in thinking, than requiring legislation.
Too many of us have been culturally conditioned to expect relief for or avoidance of “pain” that is short-lived and perhaps tolerable. If, in addition, we are motivated to wage a campaign against the folks making all kinds of money off of this, well, there’s plenty of opportunity to do so.
I gave birth unmedicated, then later popped one Tylenol with codeine. Was charged $100 for that one tablet. That was in 1986, and I’m still mad about it.
Patients in need most certainly deserve access to effective pain relief, but we may do well to consider the language available to describe it, how we improve our ability to tolerate a bit of it, and how to collaborate with a doc to say when enough medicine is enough medicine. Perhaps a system that offers credit or a refund if we return unused portions of these prescriptions??
I would greatly prefer to see the “follow the money” approach — identifying where other forces put pressure on doctors to prescribe a certain way, or why some doctors don’t have the time/training to make better decisions — than more legislators interfering in a doctor/patient relationship. Some patients have truly severe, debilitating pain. You know what makes it really hard to fight an already-complicated system that throws dozens of barriers between you and your healthcare? Debilitating pain.
People who suffer under limits on medication will be those who can’t afford another co-pay, aren’t able-bodied enough to easily go out and keep picking up 2 more days worth at a time, don’t have anyone helping to take care of them after a major surgery…people who are already disadvantaged and now have to struggle harder.
Let’s try asking doctors how to help them prescribe better, and treating addiction better.
Thank you, Will, for alerting us to what the legislature is considering. They should not attempt to solve the problem by coming up with a one-size-fits-all mandate for doctors. They should indeed legislate ways to cut down on aggressive drug marketing and eliminate ways that doctors can be given financial (or other!) incentives to over-prescribe.
+1!
Dear Will: Yes, physicians and nurse practitioners are getting it wrong. But that’s not the point — or not, at least, the sole (or most important) point.
“If they are getting the balance wrong, there is a second and distinct question: do you feel that the legislature should pass new laws regulating the decisions that doctors make with patients?”
Legislation that controls physician prescribing might help. But it is probably among the least effective policy interventions available. For one thing, it carries significant risk of unintended consequences, including some absolutely terrible ones like gross undertreatment of pain (especially post-surgical and cancer-related pain).
A more fundamental problem is that such proposed legislation (eg limiting how much or how often a physician can prescribe) fails to address the reasons why pain pill prescriptions have skyrocketed over the past 20 years. It is not because doctors suddenly became drug-happy libertines intent on doping up the American public. This is crucial, Will, and I’m very distressed to see that, aside from a few (I count two) brief asides, it is almost entirely absent from your otherwise thoughtful analysis here:
The primary drivers of the current crisis are as follows: aggressive pharmaceutical marketing, combined with the absolutely pervasive influence of the “customer service” industry, in collaboration with the health insurance industry. Physicians are under extraordinary pressure to see dozens of patients daily. Length of visit is almost never sufficient to allow satisfying interaction. In this context, the presence or absence of a prescription for OxyContin often spells the difference between a 1 and a 5. If this sounds simplistic or exaggerated, I can tell you based on my 20+ years in community health settings that it isn’t.
Another significant problem with your analysis is that it barely touches on the need for vastly increased access to addictions treatment. I was struck by the blandness of the following statement: “Availability may be more stable than need, so stability in treatment admissions may be as much related to limited availability as to need. With that caveat…” This isn’t a “caveat”. It’s a scandal. In the midst of an unprecedented epidemic, causing so much death and misery that it’s actually reversing national life expectancy trends (think about that!), Massachusetts has managed to achieve precisely ZERO increase in addiction treatment availability.
In light of the above, I’d like to urge you and your colleagues to consider the following two forms of legislation:
1. Resume the gift ban! It’s shameful that this crucially important foundation for patient and community safety (and civil rights — like the right to know how much ones doctor receives from the industry) was ever allowed to be trashed; and the current opioid epidemic is only the most dramatic of the many negative consequences of its weakening;
2. Require the state, and private health insurers, to radically expand access to addictions treatment. The only thing at will stop people from dying is treatment on demand. Why don’t we require it?
Three last things:
1. I’m confused by your opening paragraph. You describe “three intertwined problems”: episodic youth abuse; addiction in young adults; and older adults who “use or abuse pain relievers prescribed to them.” But (as you immediately go on to show in the numbers you cite), in reality, one of the most urgent problems (in terms of mortality but clearly also in terms of cost to society) is addiction in older men (45-54). Where is that “intertwined”?
2. The fentanyl issue is a red herring. The “local anecdotes” you’re hearing are just that. I implore you not to become distracted by this. This epidemic, and the deaths it is causing, are the result of OxyContin overprescribing (chiefly for non-surgical, non-cancer pain) and highly sophisticated (black-)marketing of heroin. Fentanyl is a footnote.
3. Last but not least: in 99% of clinical encounters, rational prescribing of opioid pain medication would pose no significant societal risk. It’s not rocket science: acute (post-surgical and traumatic injury) pain and cancer-related pain generally require opioids. Most other pain (chronic conditions, arthritis) does not. In your description of the relevant reports (2011 and later) of the Institute of Medicine, you indirectly acknowledge these distinctions (they specifically cite the Pain Relief Ladder for Cancer, for example; and while they speak emphatically about the need for better pain treatment, they do NOT equate this with increased prescribing of opioids!) It is important to understand this really is, with few exceptions, a bright line: narcotics for chronic pain is bad medicine.
Thanks Will for your continued attention to, and admirable work on, these difficult issues.
Yours Truly,
Jim Recht, MD
Part-Time Assistant Professor of Psychiatry
Harvard Medical School
Thanks, Jim. 100% with you on the treatment issue — more to come on this subject. Note the title of this piece as “Part I”.
I really would like to hear more about what you are pointing to when you say:
Regarding Fentanyl, I think it really is a big deal. When I talk to people doing autopsies, they say it is present much of the time, often alone. That’s in Massachusetts and the Rhode Island report offers harder numbers pointing to a lot of Fentanyl.
Thanks Will. Regarding my comment about “the difference between a 1 and a 5,” I was referring to customer satisfaction surveys, the inappropriate use of which has contributed in significant ways to this crisis.
Jim
I would really like to speak with you directly about this. I am a cancer physician and my biggest issue is making sure my patients are not in pain during their treatment. The bigger the obstacles that are put in place the harder it will be to provide appropriate care to needy patients. It is already getting progressively more difficult (prescriptions only valid for 72 hours, limited stock of drugs in pharmacies, hard scripts for all but those actively on Hospice. This puts a tremendous burden on the patient and their family having to make frequent trips to physicians and pharmacies. In my almost 30 years of practice, I have seen or suspected only 3 patients who I believed were diverting/misusing pain medications out of thousands I have cared for. I have had hundreds of legitimate terminal patients and their families struggle to get needed pain relief because of barriers. I am quite aware of the opioid crises we are facing, but cancer patients should not be punished for misuse by others.
There has to be a way to stratify legislation to identify those areas where there is a pressing medical necessity from those where opioid abuse potential is high. moreover, I would think that putting money and effort into treatment and rehab is a much better bang for the buck…legislate mandated treatment for addiction (and payment for it) in addition to restrictions and we may get somewhere!
Lisa, call me if you want to get together.
I think we can definitely can stratify, probably best through regulation — the Govenor’s proposal for a 72 hour first-time supply contemplates a set of regulatory exceptions.
I have had more than 5 surgeries over the years. After each one I was given a scrip for opiod painkillers. I rarely filled the scrips and never used them.
But here’s the thing- there was never any discussion ahead of the surgery to plan various ways to control for pain. For instance, knowing that severe pain will last one day is very different than knowing severe pain might last for many days.
There can be different strategies brought to bear such as using opiods for one day and then switching over to Motrin for the remaining days.
I think the anesthesiologist should routinely schedule pre-op appts with patients to thoroughly address the pain management. But what happens instead is a scrip given to the patient after surgery. No discussions.
The summary provides some very good data and new insights for me. There is a need for balance.
I would favor more limits on the number of pills dispensed for minor injuries. I have been given more pills for pain than I needed, more than once.
I think the risks of developing opioid dependence exceed the inconvenience of returning to a doctor for more medication if pain persists. The misuse of unused medication is another risk.
No point in my adding to the many informed and cogent comments except to say that legislation by those uneducated in medicine and influenced by public anxiety is much too broad a brush to use on this medical problem. It can and should be dealt with within the medical profession by whatever means they devise. Effective doctors are already overburdened with legislated and insurance-connected problems. One of the real questions that needs to be addressed is why so many people feel such need for relief of whatever problems they have that they buy or steal drugs. That gets us into economics and psychology. Until the problem is better defined, legislation is useless.
Dear Will,
Thank you for seeking input on this issue.
I have a son who has mental health issues and has almost died from addiction. He’s also experienced homelessness. That’s one side of the equation. What’s being almost completely overlooked in this discussion is the plight of many people like me who suffer from significant chronic pain issues. In my case a joint disease in childhood caused significant damage.
Personally I hate pain meds. They give me nightmares, upset my stomach and generally make me feel uncomfortable. I can tolerate one-quarter of one pill. That’s it. But the times when acupuncture, massage therapy and chiropractic treatment can’t get me to sleep at night, thank God I have a few pain pills I kept after my most recent surgery because according to my PCP the MA legislature has made it so difficult for her to give me a prescription she doesn’t want to have to deal with it. Opioid abuse is not my fault. It has nothing to do with me personally and yet I’m lumped in with the unfortunates who abuse pain meds and have become addicted or worse. What does the Legislature suggest for people like me?
Barbara, I’m not sure what the answer is, but I do know you are not alone in this kind of experience and concern.
I hear a lot of stories about overly cautious doctors who do not prescribe pain medications to people who desperately need them. The correlation between pain medication and heroin use is just that … correlation, not causation. Most of us who have used pain medication have not used heroin. Ditto on marijuana. Correlation is not causation, and it is a mistake people make over and over again. I do not think that the legislature should be regulating the doctor/patient relationship.
Rather than blaming doctors for the opioid epidemic, I think medical professionals with expertise in addiction should be in the lead in deciding a course of action. We put together task forces and working groups with sheriffs, police, politicians, and so on. If there is a medical professional or two in the group, their suggestions are incorporated in the final report but rarely implemented. When Portugal put together a strategy commission 15 years ago, EVERYONE on it was a medical professional or academic with a specialization in addiction. In recommending decriminalization (NOT legalization, but decriminalization) for personal use, they were able to move all the financial resources tied up in arrest, prosecution, etc. to social services. That is what is needed here. Someone has to be brave enough to start the conversation, whether or not this is determined to be the best course of action for our state. And medical professionals need to be front and center in the conversation.
In my opinion,physicians should be the only ones making the decisions about patient care in reference to prescriptions for pain medication. I believe it is a dangerous proposition to have the legislature involved with patient care.
Simple question!
Why does the United States provide $18.1 billion taxpayer funded dollars to Afghanistan, which is the largest amount to any foreign country, which allows this country to supply 93% of the illegal heroin on the street killing our children? Our tax dollars are fueling the euthanasia of our future!
Actually, most of our heroin comes from Latin America. Afghanistan is a the world’s leading supplier, but their stuff does not generally reach our markets.
Drug Enforcement Agency, 2015 National Heroin Threat Assessment Summary
Washington Post.
DrugPolicy.Org
Office of National Drug Control Policy
UNODC.
I don’t have personal experience with this issue, but it seems a better issue to have doctors deciding than law (but prosecuting unethical doctors). Your country has a long history of unsuccessfully trying to address addiction issues with law in ways that create further problems. In computing we having a saying, “X was causing me a problem so I did/used Y. Now I have two problems.”
In this case maybe the new problem you possibly create is to interfere with legitimate use. Marc Goldfinger of Spare Change news wrote about this a month or two ago. He has direct experience with heroin addiction. Maybe you should seek out his opinion.
I’m surprised at the age group, 45-54, with the highest death rate. I think this should be more talked about- we seem to assume that it is younger people.
Doctors could be trained to prescribe less (the book ‘Being Mortal’ has a lot to say about this). Laws are hard to write well, so I always hesitate to put every burden on the legislatures.
I am a health care provider, who prescribes controlled substances in skilled nursing facilities. When people come in for rehab after orthopedic surgery, for example, I need to manage their pain so they can preform need exercises and return home as soon as possible. I work with each individual prescribing pain medicine to make their rehab process successful. As their rehab stay progresses, they get stronger, more independently with less pain. The pain meds are tapered down then discontinued or continued occasionally as need for break through pain. However, a small minority of people enter this process with a medication dependency. Unlike the typical rehab person, they do not have the ability manage their pain. They typically ask for as much pain medicines as possible. Trying to taper their pain medicine dosage is difficult, but doable. They complain a lot and want to go home as soon as possible. They typically are seen by various disciplines to assist them with their rehab and dependency.
In my setting practitioners are very aware of the risk of harm and dependency on control substances. We seek to improve people’s wellbeing while doing no harm. “Getting the balance wrong”, I cringe at the simplicity of those words. Drug dependency needs an holistic approach verses Mr Baker’s bandaide.
My own experience, post surgical, was that pain meds are too casually prescribed in too large an amount.
However, I am a strong supporter of palliative care, including the use of opiod pain meds. Better physician education and prescription tracking (to eliminate the physician who prescibes for money) may help. I’d also get the insurance companies involved. We pay them a lot of money, let’s put them to work on it.
Pain medication and use of such drugs as heroin should not even be compared, one is used to control chronic pain. They should not even be put in the same class. go after the drug dealers and the Mexican cartels where the real problem lies. The real problem is the illegal drugs such as heroin.
Thanks for your thoughtful and concise summary of this pressing social issue. If you’re seeking our personal experiences, I’ve had several surgeries over the last few years at Brigham & Women’s, and at each event was given only a few days supply of potent pain medication, most of which I did not use. Would rate this as an appropriate balance.
Nowhere in your paper do you deal with the ramifications of your position on people like me. I am a 68 year old woman with a degenerative spine, scoliosis and stenosis. I have arthritis and have undergone 4 joint replacements. I am in chronic pain. The pain clinic, which has seen me for 7 years, gave me opiates to ease my pain after 3 years of trying everything else. I have a computer in my belly that is hooked up by wires to my spinal cord that sends impulses to my brain that tells it that my back doesn’t hurt. I have been taking opiates for 4 years. The same dose. I keep them in a locked closet. I have never sold them or given them away. I feel no pleasurable feeling nor do I feel craving. What I do feel is relief from my pain. There are a lot of people like me, who are responsible adults using narcotics for pain. I don’t know about these doctors who give out large quantities of pain medication. I certainly have never met one. All my pain medications are controlled by the pain clinic and I have random urine screens to check that I am not using illegal drugs or prescriptions from other doctors. Yet with all this carrying on about prescription medications being the cause of heroin deaths (the connection I fail to see), chronic pain has become a stigmatized condition. The drug store pharmacists that don’t know me well treat me like a drug seeking addict. Am I one of those people who lure teenagers to perdition with my medication? I have enough problems without stigma from chronic pain. Whatever restrictions are put in place, whatever pressure you put on doctors not to prescribe, there must be allowances made for the 100,000 people with chronic pain who use opiates safely and legitimately. We suffer enough. Do no harm, Mr. Brownsberger.
Hear, hear! I see all this drum banging about the “opioid crisis” as an expansion of the failed War on Drugs that will steamroller over people with chronic pain, who are already stigmatized by society, and poorly understood by the medical profession. The legislature should not be allowed to hamstring doctors and second guess their professional opinions on how to treat pain.
Mary, thank you for speaking out — you are not alone and the voices of people in your shoes are being heard.
Well said Mary, people don’t understand how it is to have chronic pain, why take away something that helps, personally I don’t see any connection to the heroin crisis, would they take away Tylenol. Because it helps your headaches, The government should not be involved in deciding what helps individuals who don’t abuse medications and only use them to control the pain.
i had pain in my back and left arm that should have been addressed in a hospital. my doctor at the time had lost 2 out of 3 medical assistants and the one was obviously overworked and stressed out. when i called several times that day because of the pain, i was not called back until the next day afternoon. the doctor prescribed me predisone a steroid narcotic but was unavailabe to speak to me about the use and precautions.being that i was diabetic i took more than i should because i could not stand the pain and i was getting no relief. because of that my sugars spiked up to the point that i got major infections and almost died. as a result i had to have an amputation. this is just an example where certain unforseen circumstance can happen where a medical office staff and doctor cannot provide the time for the proper info and follow up help for thier patients so therefore i completely agree that the issue with all kinds of drug and prescription drugs are getting to overwhelming now that more and more americans are getting healthcare more and more without the proper supervision or follow up. since hospital care for everyone for everything is not an option, i think there should be qualified support like a nurse on the phone and for visits funded by the drug companies and regulated by your state and or federal goverment.
Thank you. As people are moved out of hospitals more quickly, I do not doubt that in some instances there is a lack of necessary support and follow-up. This is a big issue.
Dear Will,
I have read a number of comments below and agree with many commenters that heroin should not be lumped in with legitimate and necessary use of opiates for pain. Heroin and other similar drugs are not prescribed by doctors as far as I know!
Legislators need to be mindful of those who hurt all the time.
First,
I agree with Governor Bakers proposal. It is reasonable.
As a Chiropractor, it is time that the first two weeks of anyones pains due to neck or back be Conservative Care and that care could be Chiropractic, PT, acupuncture and or massage. Doctors should be required to offer conservative care first.
Second, there should be a State registry of drug prescriptions that all doctors HAVE to check to see if someone is doctor shopping for more pills before it is prescribed or pharmacies can check before pills are distributed.
Doctors are NOT taught much on pain in medical school and I have heard this from many physicians and even a doctor went on TV and was just told to just prescribe Opiods. They must be re educated to treat conservatively first. People can manage. This paradigm is a little different for only CANCER patients where pain management is more imperative.
Also, there must be a mechanism for pharmacies to take back unused pain meds so not so many are lying around peoples homes.
I think the Governors bill is a reasoned bill and should be supported.
Thank you, Peter. What’s your take on the effectiveness of the database we do have?
Point one: Make sure Narcon is legally available to a wide variety of people who may be first responders, emts of course, school nurses, possibly police and firemen, homeless shelter personnel, walk-in medical servicers such as CVS etc.
2 Strengthen social services for addicted people as one hears “An ounce of prevention is worth a pound of cures.”
3. After 3 recent surgeries, I was given pain medication that was much larger than I needed. In fact I really only needed to take one dose after each surgery. There is a problem with these prescriptions though. That problem is having to wait one day for the order to be filled. Since the script is generally given at discharge and one is likely to need that medication immediately, having to wait a day is quite troublesome.
As a health professional I strongly agree that there is a prolbem that has been growing for years. I think doctors must be educated regarding opiate Rxs and the proper use for them. We also must help those who are addicted. Strong guidelines must be followed and strategies to reduce this problem must be developed and followed.
Pat Gold R.N.
I had a tooth pulled and was prescribed a opiate based pain killer. Seeing what is going on I decided not to have the prescription filled. I did tolerate the pain and it did subside. My situation was borderline trivial. I think with these dangerous drugs, there should be a new medical discipline of pain management involved when prescribing opiates
Dear Senator,
Thank you for performing due diligence on this issue.
My husband recently had day surgery at the Brigham and 20 oxy pills were prescribed, he had no need for them, now we need to safely dispose of them which is not easy to do. He also works for a life sciences company that delivers cannabis testing equipment. We are not cannabis users, but there is a plethora of research on the human endocannabanoid system and how cannabis is highly-effective in treating pain, cancer effects and many maladies without the addictive effect opiate substances Prescribed for the same. Is a solution to transition addicts and others seeking pain relief to cannabis (which can be prescribed in liquid form)? My suggestions are:
1) research the opiate usage/death statistics in the 4 states where recreational marijuana is legal. Has access to cannabis decreased people’s use of more highly-addictive substances?
2) McLean Hospital and MGH have addiction specialties. MGH and other prominent hospitals have doctors prescribing medicinal marijuana for a plethora of pain, anxiety and cancer side-effect relief. What is the medical community saying about medical marijuana treatment therapies? What are the results? How can the medical community shift to prescribing cannabis instead of opiates? Wouldn’t this benefit the insurance system too, much lower costs?
3) living in the Back Bay, on the edge of the South End, we routinely see drug deals in the St Botolph neighborhood, and there has been an uptick in drug-related crimes and 3 shootings in the last month. The neighborhood asked for increased foot patrols, seems the police can step drug task force teams to cut off deals and suppliers.
Thanks, Nancy B. I did notice that the head of the National Institute on Drug Abuse recently suggested that a cannabinoid compound might become the pain reliever of the future.
I do volunteer work that brings me in touch with lots of people with chronic pain. Few of my clients would agree that we need to reduce the availability of pain medication. Plus I have like most citizens been a witness over the past several decades to the government’s struggles with drug control, and the lesson I draw from that experience suggests that transferring power from doctors to state officials is asking for trouble.
This is somewhat related: Seniors in the hospital, are being given these pain relievers, even though an over-the- counter med, like Tylenol, might be enough. Sadly, the side effects for opioids in some older folks can look like dementia, leading care givers to take other, incorrect, actions.
I believe an INFORMED CONSENT law would help shine light on the long- and short- term effects of all pharmaceuticals.
In loving memory of my amazing cousin Craig, who died on December 11, 2015, I humbly suggest reading Robert Whitaker’s book, Anatomy of an Epidemic.
Here’s to your cousin’s memory.
have you or your loved ones ever experienced the pain of fibromyalgia or post polio syndrome (pps)?both incurable.some victims are being denied relief because of the opiod scare. a knee jerk reaction to legitament need.
I am an epidemiologist, and I saw another epidemiologist from Massachusetts present. In her presentation, she declared she was an ex-heroin addict, and told the personal story of trying to refuse a prescription for a narcotic following surgery on her foot in Massachusetts. She had to fight with the doctor to stop her from writing the prescription, and she still wrote it. The epidemiologist reminded the doctor that she could be sending her down a slippery slope that could end in her death, but the doctor just couldn’t hear what the epidemiologist was saying.
I think public health should give doctors some evidence-based recommendations of who *NOT* to give painkillers to – like this lady. Or maybe to prescribe only a small number of pills if patient lives in the house with young people who could steal them.
Practical, evidence-based guidelines would be an easy place to start. But unfortunately, unless there is political will in the form of funding from the state to research and set up these guidelines, however, I don’t think they will happen. The drug companies sure don’t want them!
I would like to note the problem of individuals who go from doctor to doctor to get pain medication subscriptions and then purchase and abuse the drugs. I personally have a sister who was able to feed her habit by doing this. This was done even when our family warned doctors about her abuse. Is there a system which prevents this?
Yes, there is a database that is intended to prevent doctor shopping — only works if doctors check it.
I had my shoulder operated on last year and in my experience, they issued just about the right set of pain meds. This is a highly personal area — people’s tolerance to pain differs significantly.
Laws can make our lives miserable even when we’re not part of the problem — I’d like share my experience with Over-The-Counter bronco-dialators. You may know them as Primatine or Bronkaid. You may also be familiar with them as decongestant cold medicine as they contain the same ingredient — Pseudophedrine.
In the last several years, these have become harder and harder to purchase. You now need a license and there are times (when the computer systems are down) that you cannot even purchase them. The reason for this is that they are used in the manufacture of methamnetamine, so laws were passed ot make the meds harder to obtain. I guess I can understand the intent of a law if I’m locked out of my medicine for a stuffy nose — I can just tough it out.
But if I’m in the middle of an asthma attack, can’t breathe and the computer at the CVS is down, you can imagine my thoughts about Beacon hill and Washington as I check into the emergency room — thanks a bunch for making my personal affliction event more hellish.
I believe that education, not legislation, is the solution here. I wold not support new legislation in this area. This is a complex area and blanket approaches like the one proposed are simply not appropriate solutions to the problem. If government want to solve this — do the hard work and educate, not legislate.
As a chronic pain patient who abides by my contract with my pain care specialist , I don’t feel legislatures and insurance companies should dictate what and how much medication should receive to alleviate my severe chronic pain.
I could easily be wrong, but I’ve long thought that we needed some cheap+boring way of supplying drugs straight from some public health arm of the government to addicts. I’d hope to avoid harm from overdoses and contaminated needles, and also hope to make it uneconomical to push opiates since the government would steal all the new customers. And obviously, make treatment of all kinds more widely available.
I’d also move towards some sort of legalization of marijuana; I don’t know that it’s that good a painkiller, but it’s very low harm compared to so many other drugs that are legal, and it might work for some people (I know there’s individual variation; I don’t get as much pain relief from opiates as other people seem to, but ibuprofen works fantastically well for me). And, again, I would love to undercut illegal markets and put pushers out of business.
If we repeat the same anti-drug measures that we’ve tried in the past, I wouldn’t expect them to be much more successful this time around.
I’m fine with legalizing marijuana. Nobody is really ready to think about legalizing the hard drugs — cocaine, heroin and meth — they really are much more dangerous than marijuana.
Hi Will,
I agree with Sam Scoppatthone when he says follow the money!
The doctors and the pharmaceutical companies in particular.
That also applies to the legislature with regard to gambling and possibly marijuana.
The FDA was skirted with the medical marijuana,now legalization looks like it is headed our way. Unbelievable to me with the current opioid crisis we face.
I appreciate the effort you have put into this and all the issues that come your way.
Thanks for sending this.
I think you did a great job bringing out the facts about opioid abuse and the public health crisis related to it. I have strong feelings about this matter even though I can’t explain all the causes of the troubles.
My slant is an historical one. When I went to medical school 64 years ago the main thing we learned was that opioids were addictive and to be avoided at all costs. Doctors took pride in their courage and ingenuity at frustrating the requests of patients for pain relief. This seems to have been a function of the Harrison Narcotics Act, now defunct. Doctors are like everybody else. They are much influenced by public opinion and rationalize their behavior to comply with it.
When I was in Seattle in 1962-67 I was psychiatric consultant to the first Pain Clinic in the US. The war on narcotics was still foremost in doctors’ minds. I saw some bizarre examples. The Federal Penitentiary at McNeil Island sent its very sick patients to the University of Washington Hospital. I was consulted in one case where a prisoner, with a long sentence for a drug offence, was to have complicated surgery on his cervical spine which would be accompanied by a lot of pain. The neurosurgeons were so afraid of postop narcotic medication for him (because of the drug offence) that they wanted to place a catheter to drip morphine into his cervical spinal fluid so he wouldn’t need to have any ordinary post-op medication. This was an inconvenient and hazardous procedure and totally unnecessary. These neurosurgeons were among the best in the country but they were part of the culture of the times. I fortunately put a stop to this. The patient had ordinary surgery meds, recovered uneventfully, and went back to his 45 year sentence.
The next thing that happened was a reform movement. Pretty soon doctors were deluged with exhortations to treat pain until it was entirely gone. The pain severity metric cartoons with pain severity faces from one to ten were introduced. Pain clinics and long acting opioids became popular. Doctors were sued for not relieving pain enough. I have never been involved with this new movement, 1980? to present? Clearly this movement has overshot.
At present the sentiment is again changing violently. I get emails from the Mass. Medical Society several times a week now, with multiple warnings and ever more elaborate onerous guidelines and time consuming bureaucratic hoops for the use of narcotics. I am grateful I have no need to write narcotic prescriptions. Academic medicine is coming down hard on Pain Clinics, even implying that opioids should not be used at all for chronic pain not connected to a terminal illness. Pain clinics shouldn’t rely on the pain scale metric as they have been doing, but no narcotics for any non-terminal pain is an egregious step backward. I have written to the New England Journal of Medicine about this and hope they will publish my letter.
Clearly doctors have been writing too generous prescriptions for post procedure and other fairly minor pain syndromes. They have done this I imagine with the idea that the patient won’t need to call back if they are suffering. This is a convenience to both doctors and patients. But it clearly is not working out. Doctors have been made very aware of this. Believe me they get it.
(Incidentally I can’t understand why it is such a big deal to dispose of unneeded meds. I don’t know if flushing narcotics down the toilet is really bad for the environment, but throwing out old medicines is not that hard to do. People need more guidance and instruction on this. Other meds than narcotics should be safely disposed of also. Often good medical care involves stopping a medicine before the bottle is empty.) But I digress! Doctors get it now! They should use the data base when prescribing narcotics except in obvious acute cases of narcotic need. They shouldn’t give 30 Percocet for an ordinary dental procedure etc.
I am absolutely sure that major legislative interventions dictating how doctors prescribe narcotics will just make doctors unwilling to prescribe them when they should. It will start a pendulum swing back to the bad old times that obtained when I was a young doctor. It is easy to ignore other people’s pain when it takes too much time and trouble to prescribe and you can feel virtuous also. People need more education about the use of medications. Tylenol toxicity is a major cause of acute liver failure and liver transplant; the FDA is just started increased warnings about the cardiovascular hazards of Nsaids, especially diclofenac. Using Tylenol and Nsaids more has its own hazards. I think that decisions about medication use should be left to the already chastened doctors. They are already reacting strongly in accordance with the social movement against narcotics.
Carl N. Brownsberger, M.D.
I totally support this well informed statement. I hope our legislature takes heed.
Thanks, Dad. Great comment.
Regarding drug disposal, the preferred approach is drop off in authorized takeback programs. In the absence of a convenient takeback program, the FDA recommends flushing opioids and certain other abusable substances. Flushing is generally not the preferred approach for other medications — camouflaged disposal in household trash is recommended by FDA and by our environmental agency.
Takeback options exist in Belmont, Watertown and at multiple locations in Boston.
I have directly known 2 people who have major drug problems. 1. A mid 30’s female who was introduced to drug use in high school. She went several years without using. Then 3 years ago she had an injury at work and began using pain killers. A co-worker referred her to an MD known for giving pain killers. Shortly after she learned that she could trade he opiats for large amounts of heroin. It took a year before her husband realized what was going on. She then began treatment but was unable to stay with it. Within months her marriage was dissolving. The husband, an artist with a modest income, began to file for divorce in order to save himself from financial ruin. She ended up indigent. When she was last heard from she was homeless, living in St. Croix, VI.
Case #2. Male about 30. College graduate in engineering. Friends described him as the type of person who is very susceptible to addiction; coffee, alcohol, nicotine, gambling. Started using drugs in.his early 20’s. Has been in treatment programs. Was arrested. Unknown charge. Lost his first job out of college. For the past few years he has been clean but is unemployed, living with his mother. Unable to find work.
I am a 59-year-old woman whose odyssey with pain began in 2004 as a result of a herniated disc that never “resolved” itself and left me with severe chronic pain in my lumbar spine as well as neuropathic pain in both legs. For several years I took far too many Aleve (8 per day) which was risky but managed the pain at an acceptable level. 4 or 5 years in, I had additional lumbar herniations and more pain, more than the Aleve could handle. My doctor prescribed Lyrica (a wonder drug for nerve pain) and T3 (Tylenol with codeine). I got another 4 or 5 good years with this treatment. Two years ago, I became symptomatic in my cervical spine as well as lumbar. The pain was more than I could bear. My doctor prescribed hydrocodone (Vicodin), explaining to me that plans were afoot through the FDA and other avenues to severely limit its use. We decided we would cross that bridge when we came to it.
That bridge now spans before me. On a daily basis I hear warnings about the opioid crisis, and I feel that I am single-handedly responsible for each and every one of the country’s overdoses. It is a sad day when people who suffer from constant debilitating pain face the almost unavoidable future of being denied the thing that can make them not want to kill themselves; take away the opioids for chronic pain sufferers and just watch the suicide rate climb.
I do physical therapy sessions twice weekly, see a chiropractor once a week, have tried acupuncture, reiki, meditation, a portable TENS unit, neck traction and a dozen other things to manage the pain. I have read and heard people say that these things alone should be able to manage chronic pain without resorting to opioids. Not by a longshot. They are a DISTRACTION from the pain – a welcome distraction, but only a distraction nevertheless. I believe that chronic pain sufferers should be put into a class by themselves. MAKE us go through a rigorous evaluation; I would welcome that. (But I suspect that even this would be difficult since personal perception of pain is so very subjective.) But please keep us out of the same breath as drug abusers. I feel for these people and understand that they have a disease. But I am not in the same category, and I don’t expect to be treated as such.
Got it. You are not alone. Thank you for speaking out.
I feel the need to address this situation should be a priority!!
The lives lost to young people is tragic!
Please help in eliminating this occurence, that happens on a regular basis,destroying so many families.
I have had major surgery and twice been injured in bicycling accidents. On those 3 occasions, I was prescribed oxycontin, which helped me get through. I did not become addicted, and I did not misuse the medicine. I strongly feel that prescriptions should not be restricted. Do not make restrictions for all to deal with abuse or misuse by a few. In all 3 cases, I would not have been able to go to a drugstore multiple times to refill small allotments. Do not make limitations that will cause harm to those of us who use medication when necessary and use it wisely.
While we can see there’s a serious problem with drugs, there should be other ways of dealing with the issue. Can such prescriptions be tracked and flagged, to prevent an individual from getting multiple prescriptions from different doctors and providers? What about better access to mental health services? Other options to focus on problem users vs. all users.
Thank you for your consideration.
In my experience the doctors are prescribing the narcotic pain meds even when they’re asked not to. I live with complex congenital orthopedic deformity that requires multiple surgeries, and I never wanted any narcotics, as they make me feel sick. I know myself well in regard to pain management, and I do really well just with ibuprofen or acetaminophen. However, even when I inform nurses and doctors of these fact and ask them not to prescribe me narcotics, they usually insist I take them and prescribe them. Another example is about my daughter. When she was 9, she broke her pinkie and needed a surgery. She was not in pain before or after the surgery, and we were sure to mention it, but they prescribed her a liquid opioid med anyway. We didn’t get it and tossed the Rx. When the patient is not in need of pain med and/or asks not to, they should not prescribe it.
My personal experience involves two knee surgeries with different doctors, 10 and 4 years ago, and two neck and shoulder injuries. In all cases I was not prescribed sufficient pain medication to prevent or lessen the pain immediately following the surgery (only 2-3 days of meds are needed) or to ease the pain after injuries. I was also not given the option of trying a different medication when the ones prescribed (percocet, vicodin, oxycodone) had little to no effect on me. I called the doctor’s office crying the night after surgery and begged them to let me try something different and was told there was nothing else to do except try one the counter drugs (which did not help). They would not even prescribe a single pill of ambient or another drug to help me sleep, and I was up all night bawling my eyes out. It felt like we live in a Puritan state where we are supposed to tolerate such suffering rather than be given a drug to ease it.
I needed a third knee surgery this past spring and went to a specialist in California. I explained that the meds I had tried before did not work for me. They had a whole different approach to pain management. They gave me a shot of keterolac in the knee after surgery to numb it, and gave me additional oral doses for p[ain to cover the next 1.5 days until I was seen again as a follow up. I was also given several days of dialaudid, which I only had to use at night, the first three nights. Finally, I was given five ambient pills, but again, I only needed three and never used the others. It was like night and day. The philosophy was to “get ahead of the pain” instead of waiting until I am in agony to try something (or deny giving it to me!).
I get that addiction is a problem, but the answer does not lie in denying people temporary pain relief associated with surgery or injury. Perhaps part of the answer is for the doctor to limit the amount prescribed and refer a patient who needs more to a pain specialist who is subject to additional government oversight. Also, making it easy for a patient to get rid of unused meds by returning them to the pharmacy or doctor’s office for disposal, rather than having to to to a police station.
I continue to be amazed and appreciative of your efforts to inform and consult with your constituency. You have already received many thoughtful and knowledgeable comments. My initial reaction is that the legislature, once again, is trying to solve an obvious social problem with fast-acting, simplistic answers that will create more problems than it fixes. As stated in all the comments, there are a large number of issues here, each of them requiring study groups and thoughtful legislation if needed. We may need to put more pressure on the medical community to police its own, but I am totally against the legislature putting restrictions on the medical community. I have been a nurse for over forty years. In the early days, pain medication was given out very carefully and primarily to make sure that patients were able to carry out functions needed to get well, like walking, coughing, etc. after surgery. We have now progressed to the point where there seems to be an expectation that there should be no pain. The smiley face pain charts in the hospitals that I saw with my own family members are bizarre and the fact that hospital ratings would have anything to do with that is crazy. The current crisis gives us an opportunity to have these conversations and change many things, none of which will need legislation. Modern medicine has also allowed individuals to live longer but also have incredible pain. Nothing should happen to make those individuals’ lives worse than they already are. All of us have the opportunity to tear up pain med prescriptions when they are given to us. I just wait to fill them, because I don’t want to spend the money, and then usually don’t need them. Pharmacists need to be in on this discussion, because the prescriptions could easily read: five of whatever with a specific number of refills so that there aren’t extra pills laying around. I don’t know very many people who throw those pills away, thinking that they might need them later, so there is a lot of medication laying around. Medicines should NEVER be disposed of in any water supply. They are easily broken up and thrown in the trash in the communities that incinerate the trash. I haven’t read much on medicines in trash that go to a landfill, but it sounds like a future nightmare. Instructions included with a prescription on how to dispose of the remainder of the medication would cost some money but sounds like it would be worthwhile considering the number of comments on it. The community collections of medications are complicated and expensive, and I’m guessing that it would be a nightmare for most pharmacies to have to take back the medicines. It is just too large of a topic for this comment but the lack of mental health services is a huge piece of this puzzle. Our health insurance industry loves to hand out medicine for everything, instead of actually taking the time and discussion necessary to really address the problem. Ask any mental health professional whether there are enough mental health beds or therapists to assist with these problems and they will tell you, “NO!” Thanks again for your hard work on this and other legislation.
A lot has been covered in your write up and the emails that I won’t repeat. One thing I read today is that since there is no system for informing doctors if their patient has had treatment for an opioid overdose, they often (more than 80% in one sample) continue to prescribe opiates to these patients. This could be addressed by additional legislation/regulatory changes. Also, the few times I’ve had a patient who abused the meds I prescribed (in my case stimulants since I don’t prescribe opioids) there is no way,without a patient’s signed consent form which you’re not likely to have, to warn other doctors in the patient’s pharmacy profile/Prescription Monitoring Program that an alert has been raised. Different pharmacies handle it quite differently- some legislative/regulatory clarity here could be helpful too.
Good points about the systems, Naomi. Thank you. I will pass them on.
I have been taking opioid pain medication for about sixteen years . With out it I would have ended my life myself . With out it I would not have been able to take care of myself or my children. Doctors should not have to fear treating people in pain.we need new medicines to treat pain not polititions making medical decisions for us.
New meds may be a big part of the solution.
1. When people don’t have access to primary care physicians, they hop from one ER to another trying to get opioids and ER doctors can’t refer them back to anyone so they give in and give them pills.
2. When hospitals must make money, ER doctors get bad customer reviews if they don’t give people opioids even if the people would be just as fine with something like Motrin.
3. Cities like Pittsfield don’t have enough police on the force to properly counter the influx of drugs. Heroine is now cheaper than many prescription drugs and it is easy to sell it on under-policed streets.
Yes, I think this customer review issue is an important part of the problem. Customer feedback is terribly important, but how it is framed for pain medication is something that needs attention.
Senator we all appreciate your caring efforts, i agree with your position and God speed to you and us all in getting it passed.
Thank you so much Senator for addressing this issue here, where people can chime in. I need to start by saying that I have several compound chronic pain conditions, and am over 50, with many years of all therapies. I think it would be disastrous if doctors had their hands tied when it comes to chronic sufferers. I do believe that some of my conditions are derived from childhood sexual abuse, and that legislature could never tackle controlling something like that — instead, it’s more visible to tackle the doctors.
If I had no access to pain medication I would most certainly end my life at some point. I get drug tested every 2 months to ensure that I’m not abusing it, + to be sure that I’m not selling it. Doctors are not to blame here. **How ’bout a huge movement to help people who have no idea why they feel the need to an escape ??? It’s a sad reflection: people needing a license to fish, but not one to raise children. Again…doctors are not our parents and are not to blame for this epidemic. I’ve lost several friends who chose to use IV heroin, and some of them were never even claimed at the morgue. My particular friends didn’t have a very good family-base though I understand so many do/did. The focus should be on parenting and family. (But good luck with that!!). Please, please don’t take away the ability of responsible people, responsible doctors, who are trying to keep good people above water.
Thank you again Senator and keep up the great work 🙂
Thank you NTD — As I listen on this issue, I am moved more and more by the need to ask just the question you are asking: Why are people continuing to take these drugs? In some cases, it is chronic physical pain. In others, it is chronic emotional pain and hopelessness — putting our attention on those underlying problems may be most important.
I have been a chronic pain patient for a decade. I am 68 years old. When I first went to a hospital pain clinic 7 years ago, I was put through rigorous tests and procedures that did not involve opiates- for perhaps 3 or 4 years. Only when these other measures proved inadequate for me to control my pain to a point where I could continue to work and support my family, was I given opiates. Small doses at first, gradually increasing to the point where I am now. I have had the same prescription for three years and it works well. i do not need anything stronger for daily use. I have never run into these doctors who give out painkillers indiscriminately. I keep my drugs under lock and key. I do not use alcohol or other recreational drugs. My pain clinic is aware of all the drugs I take and is the only source of pain medication I am allowed to have, even post surgery. They were involved in my care when I had my three knee replacements, hip replacements, rectal prolapse and intestinal resection. Not to mention the surgeries I had to implant the neurostimulator that also serves to control my pain. Perhaps it is because I went to professionals that I have had such success, and I do consider myself a success. I am not an addict, although I am physically dependent on the medication in that I would get sick if they were suddenly stopped. But I feel no craving and I don’t exceed my dosage. The most important thing about being maintained on the opiates is that I can work as a crisis counselor and grant writer for a homeless organization. If my pain weren’t controlled I wouldn’t be able to get out of bed. I would love to continue to have a life, just like everyone else. I would be happy to testify at any hearing or speak on the topic if it would help.
Sounds like you are doing everything right.
The law is not intended to make pain management harder in chronic situations and I don’t believe it will.
As I get older – I’m 68 – I think about a time when I might move from my current address to something smaller. This would probably be a move to a smaller town or area away from my pain clinic where I would have to rely on the services of a PCP. I would bring my record etc from the pain clinic and make sure they were in touch. But if you make it so that a regular doctor could not prescribe my medication, then I am stuck in my current address regardless of whether I can make the stairs to the second floor- a frightening thought. You guys could really ruin my life. Please see my previous comment.
I think the rule is intended to preserve the latitude physicians need to care for chronic pain.
I’d be very concerned if we didn’t do that.
Who will monitor and insure compliance? In recent months, we have witnessed nurses working in healthcare without the proper licensing or credentials! EMT and Paramedica toiling without updated credentials and worse yet, the failure of cities and towns emergency responders meeting established critical response times! Without the teeth of strict compliance, this is just mush!
I think that doctors take the law seriously because their livelihood depends on avoiding legal complications.
Stick to running the state and stay out of the medical profession. The Commonwealth can not even take care of the children under it’s care right now and has deficit – people will always abuse something
I agree that we should be careful about what we take on. This is a relatively modest step.
Any opiate prescription should be documented in a universal data base, available to doctors, pharmacies, and regulators, to prevent individuals from “shopping around” for a doctor who will, unknowingly perhaps, fill that prescription without knowing that person’s medical history.
Soooo… the only real purpose of this law is to encourage practitioners to issue only 7 day scripts, but if they think they need more than 7 they need to additionally document it. On the face of it this seems like reasonable best practice, but I question why this [[needs]] to be a law.
I just switched insurance coverage and have been without my blood pressure meds for about 2 weeks while they straighten out bureaucratic stuff. I shudder to think what this would be like with the legal aspect to wrangle with.
Once again, I will suggest the solution to these problem is education, not legislation and urge you to “Just Say No” to this law.
I agree that education and culture change is the hear of it. But law making can be part of that process.
The state should improve the tools it provides to physicians to monitor opioid use. The Department of Public Health’s Online Prescription Monitoring Program website is very useful. It allows physicians to look to see what opioid prescriptions the patient has filled within the past year. However, there is a delay in data transfer. One of my patients filled a prescription on 1/2/2016, and the data still aren’t in the database. The information should be transferred overnight.
Definitely an area for improvement!
Thanks Will for taking such a measured and thoughfull approach to this complex problem.
It is noteworthy in your reprt that the vast majority of diverion occurs between friends and family from medication obtained from a single doctor. Many doctors now require patients to come in for random pill counts to try to eliminate diversion, but this is quite time consuming for already very oveworked doctors and staff, difficult for some patients, and can be gamed once people are aware of the process. As you noted there has been a drop in the past 2 years as doctors strive to find a balance between treating pain and ensuring prooper use of medications. In the end,however, doctors can not control what people do with the medication that is prescribed. Patients also bear equal responsibilty for using medication responsibly. (Perhaps there should be a law about the transfer of controlled sunstances to friends and family ?)
Doctors are not omnicient and and are not the police or the DEA.. There is a price that is paid for the increased vigilence of the medical community. Every minute that we spend on opiod monitoring is a minute that we take away from some other task that may be equally important.
My only suggestion would be that improved communication between health care insitutions doctors, pharamies, mental health providers. Primary care doctors should recieve electronic notification when our patients fill prescriptions for controled substances -The state precription monitory progran is good – but it still takes 5 minutes to go to a website- log on remember a pasword, enter the patient information. The state should mandate that all major electronic medical record systems “talk” to each other- so that when a patient is seen at another hosptals ER with an injury and needs pain medication doctors can find out in real time what test were donne and what medication was prescribed.
HIPPA – the law which regulates privacy-specifically states that communication amongst health care providers needed for that care of the patient should not be impeded. However fear of being accused of violating HIPPA ( which is very expensive ) definately impedes communication needed to properly care for patients with chronic pain, substance abuse – as well as many others.
Many people who suffer from chronic pain also suffer from mental illness. (this can be caused by the pain or be independent)The very high wall that is in placed between mental and physical health providers makes coordination of care for these patients extremely difficult.
Many non opiod medications used for nerve ( neuropathic pain ) are also used for teatment of anxiety, deprssion, and mood disorders. Mental health providers are even more overbudened than primary care doctors and often have neither the time nor the inclination to work as a team on issues of pain control. The fact that we have segregated mental health care from the rest of health care exacerbates this problem. Many patients must obtain their care from community mental health centers which are very overburdoned. Communication is virtually impossible- hence optimizing most patient’s treatment is a daunting task.
Thanks again Will for taking the time to understand the complexity of this issue and for supporting a reasoned approach to a very difficult problem.
Barry
Thanks for these thoughts, Barry. Your point about systems integration and communication is very well taken. I hope we are able to improve this — your point resonates very much with Dr. Meyer’s point below.
BTW, anyone giving pain meds to a friend or family member is committing a felony — it’s just so private that it is not enforceable.